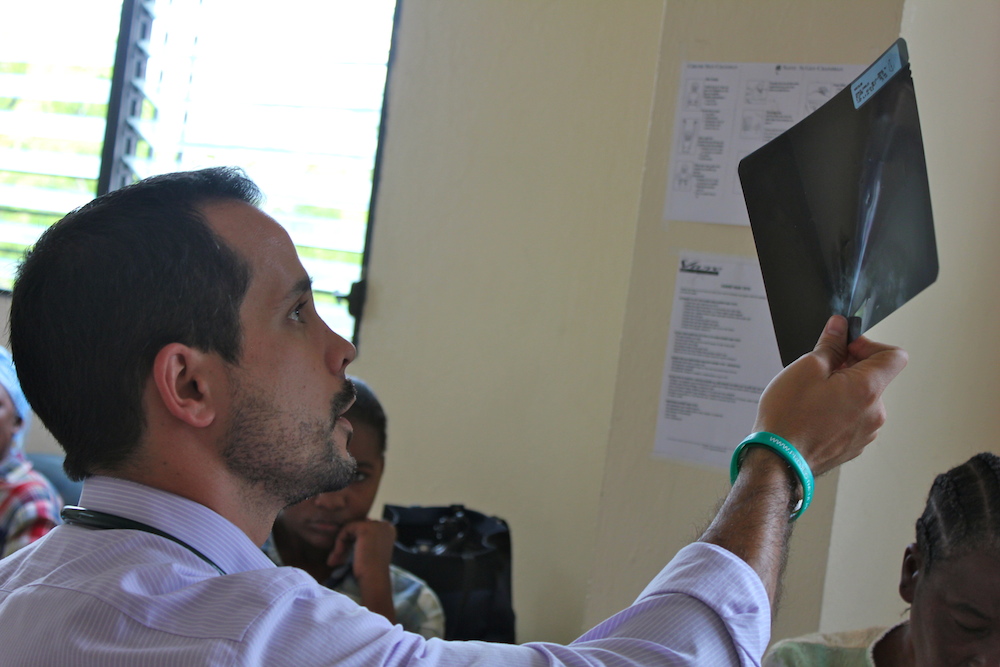
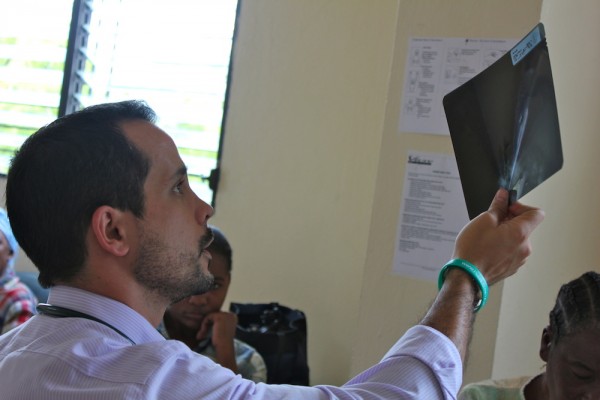
Antoinette is only 38 years old, but she has advanced-stage breast cancer. By the time I met her at the Project Medishare hospital in Port-au-Prince, Haiti, the tumor had eroded the skin of the breast, creating a foul-smelling wound.
The tumor in her right breast had grown for two years before she acknowledged it would not go away on its own. Doctors in the United States often require mammograms, ultrasounds, and repeated biopsies for diagnosis. Doctors in Haiti diagnose breast cancer before a woman removes her bra. By the time Antoinette sought medical care, the tumor was larger than the whole healthy left breast.